How do we get kids back in school and prevent them from getting COVID during the Omicron surge?
“Students benefit from in-person learning, and safely returning to in-person instruction continues to be a priority.”
Guidance for COVID-19 Prevention in K-12 Schools
After all, that’s what everyone wants, right?

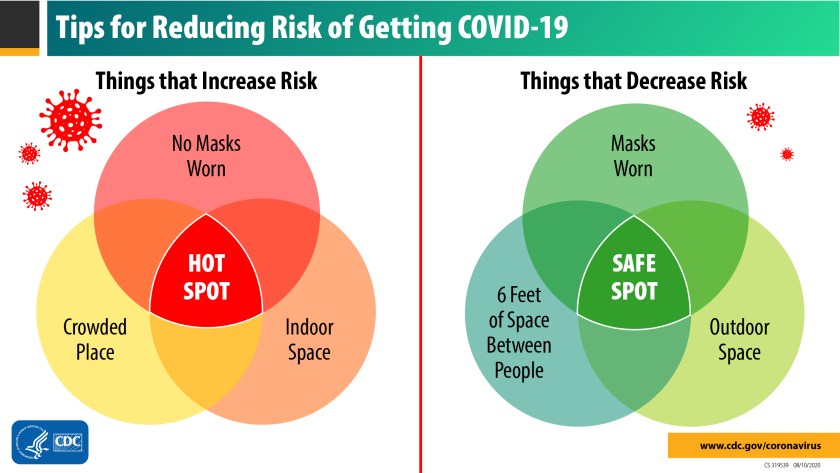
It’s hard to see how we can do that safely without a lot more people getting vaccinated and boosted, masking, practicing social distancing, more testing, and following through on quarantines for those who are exposed, and isolation for those who are sick.
“CDC recommends universal indoor masking by all* students (ages 2 years and older), staff, teachers, and visitors to K-12 schools, regardless of vaccination status.”
Guidance for COVID-19 Prevention in K-12 Schools
Still, in most cases, folks don’t want to go back to on-line schooling, especially for long periods of time.
So to get kids back in school during the Omicron surge, parents, students, and staff should all work together to keep their kids safe and healthy by:
- going into home quarantine if they have been exposed to someone with COVID and they are not vaccinated (including a booster dose if they are at least 18 years old and are eligible) or have not had COVID in the past 3 months, remaining in quarantine for at least 5 days. After 5 days, if they have not developed symptoms of COVID, they can get a COVID test and if it is negative, they can return to school, wearing a well-fitting mask for an additional 5 days. And of course, they should get tested if you develop symptoms at any time during these 10 days. If they can’t get tested after 5 days, they can still leave quarantine early if they don’t have symptoms and will wear a mask for another 5 days.
- going into home isolation if they have COVID, remaining in isolation for at least 5 days, with the ability to end isolation after 5 days if they are fever free for 24 hours, have either had no symptoms or improving symptoms, and will wear a mask for an additional 5 days whenever they are around other people.
- keeping away from anyone who is at high risk for severe COVID disease until the full 10 days of quarantine or isolation ends.
- maintaining adequate distance from others during times when they have to take off their mask at school and they are still within the last 5 days of your quarantine or isolation, like when they are eating lunch.
And what if they can’t or won’t wear a mask consistently and correctly and are in quarantine or isolation?

Then they should finish out their full 10 day quarantine or isolation at home!
“Staying home when sick with COVID-19 is essential to keep COVID-19 infections out of schools and prevent spread to others.”
Guidance for COVID-19 Prevention in K-12 Schools
What else does the CDC recommend to help keep kids in school safely?
“Vaccination is the leading public health prevention strategy to end the COVID-19 pandemic. A growing body of evidence suggests that people who have completed the primary series (and a booster when eligible) are at substantially reduced risk of severe illness and death from COVID-19 compared with unvaccinated people.”
Guidance for COVID-19 Prevention in K-12 Schools
In addition to vaccination, quarantine and isolation strategies, the CDC recommends consistent and correct mask use, physical distancing, screening testing, improving ventilation, handwashing and respiratory etiquette, contact tracing, and cleaning and disinfection, etc.
“Recommend screening testing for high-risk sports and extracurricular activities at least once per week.”
Guidance for COVID-19 Prevention in K-12 Schools
For example, in areas of low to moderate COVID transmission, doing screening tests of kids in high risk sports and extracurricular activities might help prevent outbreaks. On the other hand, when transmission rates are high, schools should probably just cancel or hold high-risk sports and extracurricular activities virtually to protect in-person learning.
Will this work?
Many big city school districts aren’t convinced and are already delaying the start of the second half of the school year…
“With the above principles in mind, the AAP strongly advocates that all local, state, and federal policy considerations for school COVID-19 plans should start with a goal of keeping students safe, physically present, and emotionally supported in school.“
COVID-19 Guidance for Safe Schools and Promotion of In-Person Learning
Let’s hope the COVID surge ends quickly, states and school districts do more to protect our kids, more people get vaccinated and boosted, and we can get all of our kids back in school!
More on COVID School Guidance
- Pfizer COVID Vaccines for 5-11 Year Olds
- Going Back to School During the COVID-19 Pandemic
- The Latest COVID-19 Treatment Regimens
- 7 Things to Know About COVID-19
- Get All of Your COVID-19 Questions Answered
- COVID-19 Vaccination Questions and Answers
- Are Kids Dying With COVID-19?
- CDC – Guidance for COVID-19 Prevention in K-12 Schools
- CDC – Overview of COVID-19 Quarantine for K-12 Schools
- CDC – Overview of COVID-19 Isolation for K-12 Schools
- Back to School Amid Omicron Surge
- CDC – Steps for Determining Close Contact and Quarantine in K–12 Schools
- AAP – COVID-19 Guidance for Safe Schools and Promotion of In-Person Learning
- COVID-19 Resources for Schools, Students, and Families
- Long COVID under Section 504 and the IDEA
- Questions and Answers on Civil Rights and School Reopening in the COVID-19 Environment
- Helping Children Cope With Changes Resulting From COVID-19













You must be logged in to post a comment.